Abstract
Background: Diffuse large B cell Lymphoma (DLBCL), the most common non-Hodgkin lymphoma, is a clinical and biological heterogeneous entity. R-CHOP is the standard treatment, however 30%-40% of DLBCL patients will have primary refractory or relapsed disease. Several prognostic scoring systems, that include simple clinical parameters, have been developed to assist risk stratification and treatment decisions, namely the International Prognostic Index (IPI), the National Comprehensive Cancer Network IPI (NCCN-IPI) and the GELTAMO-IPI. However, the accurate identification of very high-risk patients is not accomplished by these scores. Recently, the Kyoto Prognostic Index (KPI) was able to identify an extremely poor prognostic group in a Japanese cohort and was proposed as a new robust prognostic model for DLBCL. Our aim was to assess the discriminative performance of IPI, NCCN-IPI and GETALMO-IPI in overall survival (OS) and progression-free survival (PFS) and compare them with the new score KPI, in a cohort of DLBCL patients treated with immunochemotherapy.
Methods: Retrospective analysis of HIV-negative DLBCL patients, newly diagnosed between 2010 and 2019 in a single tertiary center, treated with R-CHOP/R-CHOP-like protocol. The Kaplan-Meier method was used to estimate the probabilities of OS and PFS. Stratified models for each of the risk scores (IPI, NCCN-IPI, GELTAMO-IPI and KPI) were compared using Akaike's information criterion (AIC) and the Harrell's concordance index (C-index). The inter-score classification concordance was evaluated by Cohen's kappa test. P-value<0.05 was considered statistically significant.
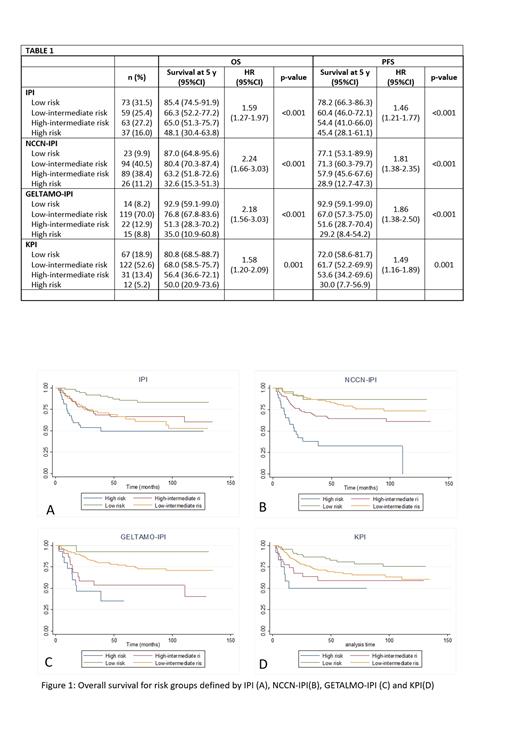
Results: We included 232 patients, 52.6% (n=122) male, with a median age of 64 years (22-87). According to IPI, patients classified as Low (L), Low-Intermediate (LI), High-Intermediate (HI) and High (H) were 73 (31.47%), 59 (25.43%), 63 (27.16%) and 37 (15.95%), respectively. According to NCCCN-IPI, patients classified as L, LI, HI and H were 23 (9.91%), 94 (40.52%), 89 (38.46%) and 26 (11.21%), respectively. GETALMO-IPI was calculated in 170 of 232 patients, classified as L, LI, HI and H in 14 (8.24%), 119 (70.0%), 22 (12.94%) and 15 (8.82%), respectively. According to KPI, patients classified as L, LI, HI and H were 67 (28.88%), 122 (52.59%), 31 (13.36%) and 12 (5.17%), respectively.
Between KPI and IPI, a fair concordance was observed (kappa 0.363; with only 10 [27%] IPI-H patients classified as KPI-H, and 10 [83.3%] patients KPI-H as IPI-H). Slight concordance was observed between KPI and NCCN-IPI (kappa 0.115; 9 [34.6%] patients NCNN-IPI-H classified as KPI-H, and 9 [75%] patients KPI-H as NCCN-IPI-H), as well as between KPI and GELTALMO-IPI-H (kappa 0.175; 6 [40%] patients GELTALMO-IPI-H classified as KPI-H, and 6 [60%] patients KPI-H as GELTALMO-IPI-H).
With a median follow-up of 55.2 months, 5-year median OS and PFS for the global cohort were not reached (NR) and 128.2 months, respectively. All the scores identify different prognosis groups for OS and PFS, although with modest ability to distinguish between intermediate and high-risk groups (Table 1; Figure 1). GELTAMO-IPI provided the best fit for the data in both OS and PFS (AIC 479.4 and 631.0, respectively) followed by NCCN-IPI (AIC 727.3 and 933.8) and IPI (AIC 738.3 and 937.9), while KPI had the worst performance (AIC 745.6 and 943.7). NCCN-IPI discriminated better between patients with poor and favorable OS (C-index 0.667), compared with the remaining scores (C-index for IPI, GELTAMO-IPI and KPI 0.653, 0.647 and 0.612, respectively). Concerning PFS, IPI had the best discrimination capacity (C-index 0.6313), followed by NCCN-IPI (C-index 0.6232), GELTAMO-IPI (C-index 0.6086) and KPI (C-index 0.5940).
Conclusions: In our cohort, GELTAMO-IPI had the best fit to the observed data regarding OS and PFS. NCCN-IPI and IPI discriminated better between patients with poor and favorable OS and PFS, respectively, although the differences in the C-index were small, and all scores exhibited an acceptable difference between short and long survival times. KPI did not seem to improve the capacity for predicting OS and PFS in our population, which could be explained by differences in pathophysiology and genetics of DLBC of Asian and Western patients. Novel risk scores that integrate molecular tumor features might help improve risk stratification, especially in high-risk group.
Gomes: Takeda: Consultancy; Gilead: Consultancy; Janssen: Consultancy.